Even if the insurance company denies a procedure, such as an MRI, don’t take their answer as final. Speak with an experienced St. Louis car injury lawyer.
FREE CASE EVALUATION
Uninsured motorist coverage protects Missouri drivers involved in car accidents with drivers who do not carry the mandatory auto insurance, or if they are the victims of a hit and run.
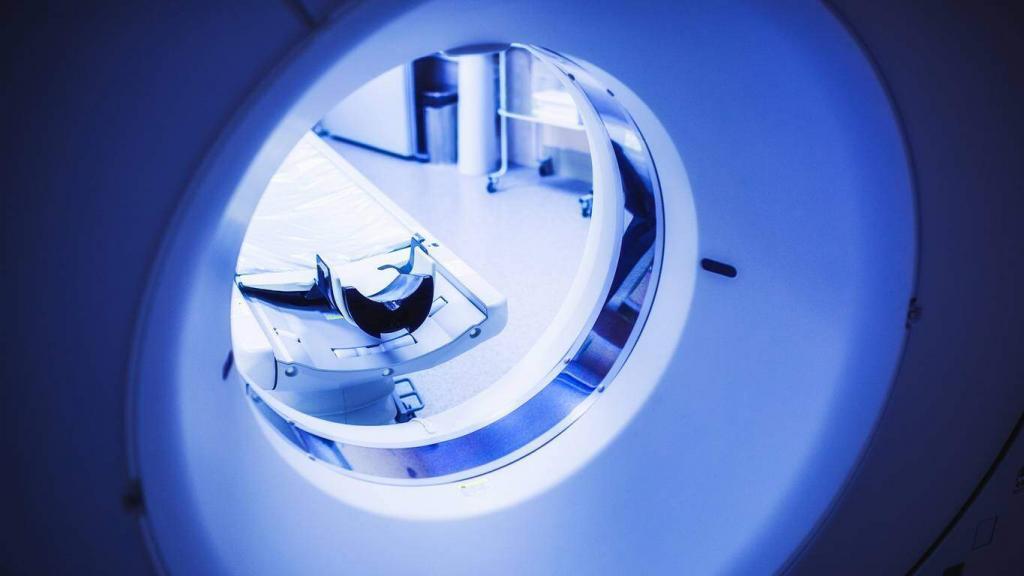
Apart from the standard auto insurance, Missouri also mandates this uninsured motorist coverage to increase your protection while driving in the state. However, is this coverage enough when you need very expensive procedures, such as an MRI?
How the Uninsured Motorist Coverage Works
In Missouri, this insurance policy is set at a minimum of $25,000 per person and $50,000 per event. Your uninsured motorist coverage will generally only come into effect when you are in a car accident and the at-fault driver lacks proper auto insurance, or when the at-fault driver flees and is nowhere to be found.
If you’re the victim of either of these scenarios, your uninsured motorist coverage should cover the cost of your medical bills as long as you do not exceed $50,000, which is your total coverage per event. If the bulk of your medical bills exceed it, the insurance company may refuse to pay.
This poses a big problem for drivers (or passengers in the vehicle at the time of the accident) that have extensive injuries that require more expensive investigations, such as MRIs. The average cost of an MRI is around $1,000 – $2,000, without accounting for doctor fees. If you also need other expensive procedures, it can easily go over the $50,000 limit.
The Insurance Company May Also Refuse to Pay, Even If You Have Good Coverage
There is another issue with expensive, investigative procedures like MRIs. You have the right to purchase better coverage if you choose to, meaning you may have insurance that goes over the $50,000 state minimum. But even then, the insurance company can deny paying for an MRI.
This may happen especially if the procedure was done without prior approval from the insurance company, like if you were rushed to an MRI because your doctor thought it was the best procedure at the time, but did not wait for approval. The insurance company may argue that all you needed was a cheaper procedure, such as an X-Ray or a CT scan, which are much more affordable.
Even if consulted beforehand, the insurance company may still ask for an X-ray or CT scan first. Only if these results are inconclusive will they agree to an MRI.
When it comes to other procedures, it may be a matter of whether the insurance company believes they are truly necessary. Of course, since they are not medical experts, their opinions on your treatment should not matter, but in some cases, they may affect your claim.
What Can You Do?
Even if the insurance company denies a procedure, don’t take their answer as final. Discuss your car accident with an experienced St. Louis car injury lawyer to ensure your legal right to compensation is protected.
Why Choose Us vs TV Lawyers?
Direct Attorney Access
Maximum Settlement Focus
Trial-Ready Cases
Paralegal Handling
Quick Settlement Push
Settlement-Only Focus
Free Consultation with a St. Louis Car Accident Lawyer
Don’t talk to an insurance claims adjuster before speaking with The Hoffmann Law Firm, L.L.C. We can help you avoid making statements that may affect the outcome of your case. The consultation is free; you don’t pay unless we get you money!
